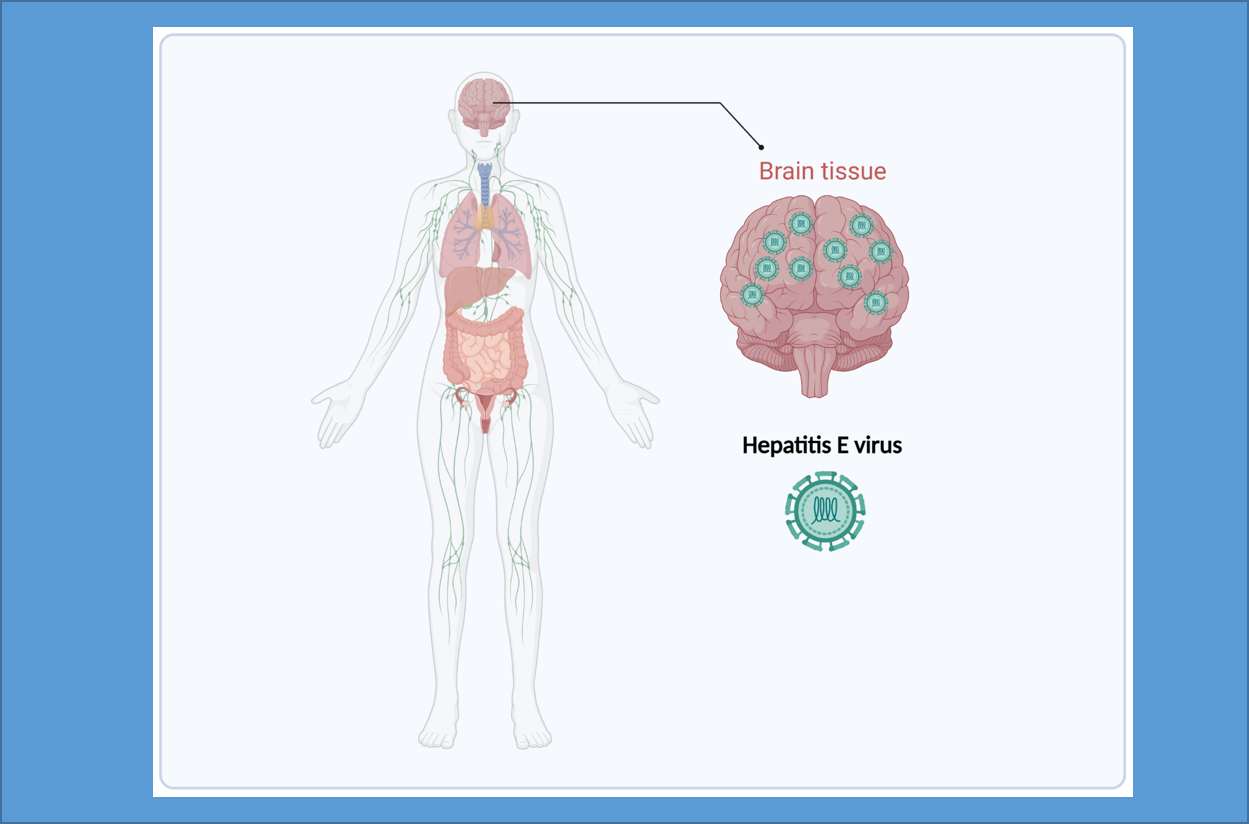
Hepatitis E virus (HEV) is the major cause of viral hepatitis worldwide. While the water borne HEV genotypes 1 and 2 are found in developing countries, HEV genotypes 3 and 4 are endemic in developed countries, due to the existence of animal reservoirs, especially pigs. An HEV infection can produce extra-hepatic manifestations, including neurological disorders, in addition to liver symptoms. The most common are neuralgic amyotrophy or Parsonage-Turner syndrome, Guillain-Barré syndrome, myelitis and encephalitis. The pathophysiology of the neurological injuries caused by HEV is unclear. The immune response to the virus is probably involved but direct virus neurotropism could also be a contributing factor.
Studies using a replicon system based on the Kernow strain, in which ORF2 is replaced by the Gaussia luciferase, showed that transfected glioblastoma multiforme (DBRTG), desmoplastic cerebellar medulloblastoma (DAOY), glioblastoma astrocytoma (U-373 MG) and oligodendrocytic (MO3.13) cell lines all support HEV replication in vitro, with MO3.13 being the most efficient. This cell line also supports the full HEV replication lifecycle. Other works with several animal models, including Mongolian gerbils, rabbits, mice and rhesus macaques, detected the negative RNA strand, an intermediate of HEV replication, and/or ORF2 protein in the brains of these animals. Thus, HEV can infect the brains of all the species tested. However, there is, as yet, no evidence that it infects human brains.
A recent study led by Dr. Sebastien Lhomme and Prof. Jacques Izopet reported a case of a 69-year-old chronically HEV-infected woman who was given a haploidentical allo-hematopoietic stem cell transplant. After diagnosis, she was treated with ribavirin 800 mg/day. The neurological disorders appeared 27 days after ribavirin initiation. Her electroencephalogram was slowed and magnetic resonance imaging showed non-specific peri-ventricular leukopathy. There was also HEV RNA in her cerebrospinal fluid (CSF). Ribavirin therapy cleared the HEV RNA from her blood and stool after 86 days but the neurological symptoms persisted and HEV RNA was found in a new sample of CSF. Analysis of the HEV quasispecies by deep sequencing showed compartmentation between the blood and the CSF, together with evolution of the CSF quasispecies. These data suggest that HEV replicates autonomously within the central nervous system but the CNS cells targeted by the virus were not yet identified. Physicians should not overlook neurological symptoms due to the virus in apparently cured patients with a recent history of HEV infection.
Read the full article (J Antimicrob Chemother. 2022 May 10;dkac147) https://doi.org/10.1093/jac/dkac147.
The featured image was drawn using BioRender.