Organ transplant recipients with hepatitis E virus (HEV) infection bears high risk to develop chronic hepatitis, which is generally associated with immunosuppressive therapies. A research group led by Dr. Yijin Wang in Southern University of Science and Technology, Shenzhen, China performed a large retrospective study to investigate the prevalence of anti‐HEV at baseline, incidence of de novo HEV infection after transplantation, and the risk factors of HEV infection among patients with liver transplant in China. A total of 407 liver transplant recipients were examined for the presence of anti-HEV immunoglobulin G (IgG), IgM antibodies, and HEV RNA in serum. All of them received tacrolimus, among which 340 received steroid as well, 306 received additional mycophenolate. The follow-up time after transplantation varied from 7 to 4352 days, and the median was 383 days. 27.03% of patients received rehospitalization for graft rejection during the follow-up.
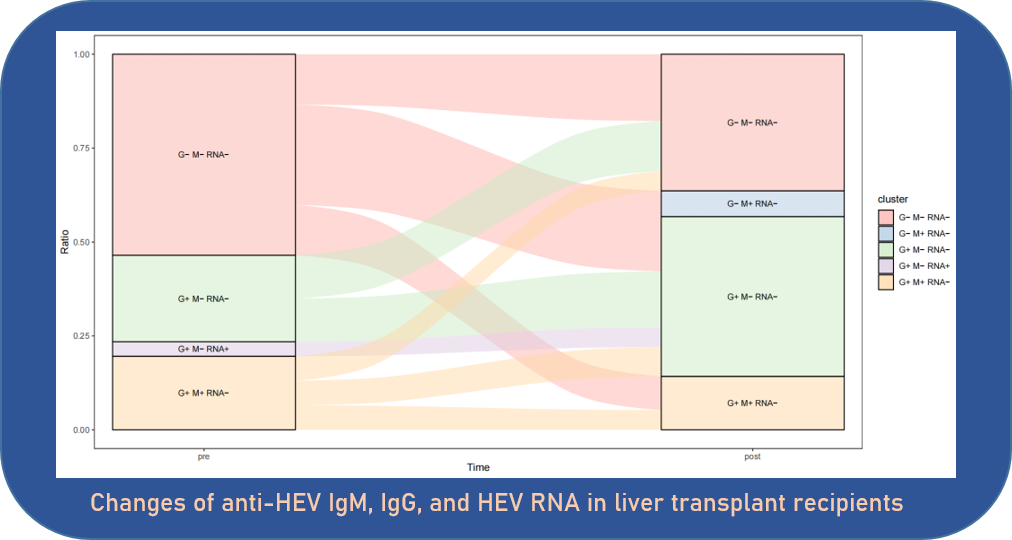
Overall, 302 patients (74.2%) were negative for anti-HEV IgG, anti-HEV IgM and HEV RNA before transplantation. 105 (25.8%) cases presented anti-HEV IgG positivity, of which five patients were also positive for anti-HEV IgM, and one patient had detectable HEV RNA with negative anti-HEV IgM. Among 302 patients with negative serum before transplantation, de novo HEV infection were found in 65 individuals after transplantation, with a cumulative incidence of 42.74% during follow-up. Of note, the seroprevalence rates dramatically increased in the first follow-up year after transplantation with a ratio of 19.35%, but kept at low infection risk between the second to fourth follow-up year. Subsequently, a gradual increase in incidence was observed from the fifth to the ninth follow-up year. After transplantation, HEV infection was associated with liver failure (P = 0.012), hypoproteinemia (P = 0.030) and higher level of r-glutamyl transferase (GGT) (P = 0.022) at baseline before transplantation. Graft rejection (OR 0.075; P = 0.045) was negatively associated with serum-negative conversion in patients who had positive anti-HEV antibody before transplantation. Interestingly, in terms of the usage of immunosuppressive drugs, patients received triple drug more likely to have HEV infection than those received double drug, despite the difference was not significant (p = 0.076).
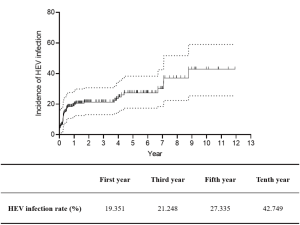
Rates of HEV infection by year after liver transplantation.
In summary, the seroprevalence of anti-HEV in liver transplant recipients is high in China. It is recommended that liver transplant recipients should avoid eating uncooked meat and avoid contact with possibly HEV infected animals. Liver transplant recipients with graft hepatitis should be carefully monitored by testing HEV‐RNA.
Read the full article (J Med Virol. 2024 Oct;96(10):e29939): DOI: 10.1002/jmv.29939