Hepatitis E is endemic in many developing countries, and hepatitis E virus is transmitted mainly by the fecal-oral route. It was estimated that approximately 20.1 million hepatitis E-related liver diseases worldwide, resulting in 70,000 deaths and 3,000 stillbirths. Although hepatitis E is asymptomatic and self-limited disease with low mortality, fulminant hepatitis can lead to acute liver failure (ALF) or acute and chronic liver failure (ACLF). About 0.5% – 4% of all acute HEV cases progress to ALF, and the rate of progression to ALF in pregnant women may be as high as 10%-22%. Notably, the fact that HEV plays an important role in the development of ALF has also frequently been reported in Europe. HEV-associated ALF (HEV-ALF) could lead to a high mortality rate of 0 – 67%. Therefore, timely diagnosis and prognosis of HEV-ALF patients are very important.
Currently, multivariate prognostic evaluation models are mainly adopted in ALF, such as end-stage liver disease (MELD) scoring model, King’s College Hospital (KCH) criterion, Child-Pugh scoring model and acute physiology and chronic health evaluation II/III (APACHEII/III) model. The MELD scoring model uses the formula developed by Mayo clinical team, collects serum bilirubin, creatinine and prothrombin time to calculate the scoring results, and predicts the prognosis of ALF. The iMELD scoring model was created in China based on the international MELD scoring system by adding age and serum Na+. The KCH criterion is mainly suitable for predicting the prognosis of ALF caused by drugs or unknown etiology. The prognosis of acute liver failure is determined by comprehensive consideration of etiology (whether it is caused by acetaminophen), PT/INR, TBil and serum creatinine. The Child-Pugh scoring model uses TBil, serum albumin, PT/INR, ascites and hepatic encephalopathy as scoring items to predict the prognosis of patients with liver disease, especially liver cirrhosis. The APACHE II/III model is based on temperature, blood pressure, heart rate, respiration rate, PaO2, arterial pH, serum Na+, K+, serum creatinine, hematocrit, white blood cells, Glasgow coma score, age, cardiopulmonary and other chronic health problems. However, the MELD model cannot accurately predict the outcome of liver failure due to the lack of clinical complications such as ascites. The KCH criterion and Child-Pugh scoring model are mainly used to assess drug-induced liver failure, while their predictive value for non-drug-induced liver failure is relatively low. The APACHE II/III model is complicated to operate and has low sensitivity for predicting liver failure. None of the above models could specifically predict the prognosis of HEV-ALF accurately. Therefore, the establishment of an efficient and high-sensitivity HEV-ALF prognostic model is conducive to the early and precise treatment of HEV-ALF patients and the prevention of aggravation.
A recent multicenter study in China led by Dr. Jian Wu, Prof. Hongcui Cao and Prof. Lanjun Li, has established a new prognostic nomogram (Figure 1). This was based on a cross-sectional set of 404 HEV-ALF patients who were identified and enrolled from a cohort of 650 patients with liver failure. Multivariate logistic regression analysis of the development set carried out to predict mortality revealed that γ-glutamyl transpeptidase (GGT), albumin (ALB), total bilirubin (TBIL), urea nitrogen (UREA), creatinine (CR), international normalized ratio (INR), and neutrophil to lymphocyte ratio (NLR) were independent factors. To further evaluate and rank the ability of the parameters to predict the mortality of HEV-ALF patients, orthogonal partial least squares discriminant analysis (OPLS-DA) was next used. Non-survivors could be unambiguously distinguished from survivors using OPLS-DA. The top 7 predictors were ln (UREA), ln (NLR), ln (GGT), ln (TBIL), ln (INR), ln (ALB), and ln (CR). UREA, NLR, GGT, TBIL, INR, ALB, and CR were finally identified as the seven best prognostic indicators, all of which were incorporated into the new nomogram to predict the mortality of HEV-ALF patients.
The area under the receiver operating characteristic curve (AUROC) of the nomogram to predict the mortality in HEV-ALF patients was 0.671 (95% CI: 0.602-0.740), which was significantly higher than the MELD and CLIF-C-ACLFS models. The calibration curve had an optimal agreement between the prognostic nomogram and the actual observation. Time-dependent receiver operating characteristics (tdROC) and decision curve analysis (DCA) showed that the discriminant ability and threshold probability were better than the MELD and CLIF-C-ACLFS models. The same performance trend was also observed in the validation cohort.
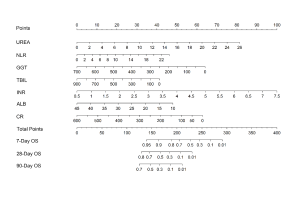
Figure 1. The nomogram for HEV-ALF patients’ 7-day, 28-day and 90-day mortality, including UREA, NLR, GGT, TBIL, INR, ALB, and CR levels. The nomogram allows the user to obtain a probability of 7-day, 28-day and 90-day mortality corresponding to a patient’s particular combination of covariates. To use the nomogram, locate the patient’s value and draw a line straight upward to determine the score received for the variable. The sum of these scores is obtained for each covariate, which is then located on the ‘Total Points’ axis. A line is drawn downward to determine the likelihood of 7-day, 28-day and 90-day mortality on the survival axis.
Read the full article published in Journal of Clinical and Translational Hepatology: https://www.xiahepublishing.com/2310-8819/JCTH-2020-00117